Snake Venom and Snakebites
by Andrew McKenzie (Originally published in Monitor Vol 13 Issue 1 2004)
Snake Venom: An Introduction
The following article has been written to explain what happens to a bite recipient if they suspect they have been bitten by a potentially venomous snake. The issues investigated are as follows;
i) How most bites occur,
ii) What to do if bitten by a snake,
iii) How venom affects the body, and;
iv) Methodology in determining whether or not to administer antivenom
Snake Venom: How Most Bites Occur
Most snake bites involve the lower parts of the body, therefore, the lower leg and foot are commonly bitten. Some bites occur on the hands. Bites can occur when poking hands into hollow logs, under rocks or under common household or farmyard shelters such as sheets of tin. Bushwalking and walking through long grass are activities which can lead to people being bitten.
 Other bites occur when people attempt to injure or kill a snake that they have encountered. The bottom line is that in the majority of cases of snakebite, the snake is only trying to defend itself. It should be noted that snakebite in domestic and farmyard animals is also a common occurrence (Mirtschin, et al. 1998), but the bitten animals again have in most situations provoked the bite by attacking the snake themselves.
Other bites occur when people attempt to injure or kill a snake that they have encountered. The bottom line is that in the majority of cases of snakebite, the snake is only trying to defend itself. It should be noted that snakebite in domestic and farmyard animals is also a common occurrence (Mirtschin, et al. 1998), but the bitten animals again have in most situations provoked the bite by attacking the snake themselves.
Snake Venom: What To Do if Bitten by a Snake
The most important thing to do if bitten by a snake is to keep calm and encourage others to do so as well so that you can focus on application of first aid and seeking medical attention as soon a possible.
See the first aid description on the AVRU web site. The PI method is thought to slow the movement of lymph in the lymphatic system. This has never been proved but there is good evidence to support it. Snake venom is thought to move from the lymphatic system to the blood stream. There are some good references on this topic (see references I have included at end). What you should not do is wash or wipe the site where the bite is, as any venom on the skin surface is useful (but not critical).
If at all possible do not drive a vehicle as you may collapse and cause an accident. An ambulance or another driver is advised. Finally, do not use drugs or consume alcohol as the effects of these may mimic the symptoms of venom in the bloodstream leading to administration of an antivenom where it is not really required. Antivenom is only given if venom is detected, or in its absence, if systemic envenomation is indicated by the symptoms.
Snake Venom: How Venom Affects The Body
 Venom can affect the body in a variety of ways.
Venom can affect the body in a variety of ways.
In general, venom appears to be a mixture of enzymes and proteins that can act on several biochemical pathways or on a single physiological pathway within the body. The effects are characterised by:
Neurotoxins:- which inactivate the nerve and smooth muscle function of the body by upsetting the sodium (Na+)and potassium (K+) channels required for neurotransmission and cardiac function. There are also ion channel blockers and inhibitors.
Cytotoxins:- which affect the cells that come in contactwith the venom, either at the bite site or in the blood.
Hemotoxins:- can either be toxins which affect haemostasis in some way (those that activate the clotting cascade, or inhibit its activation). Also there are toxins which cause haemorrhage (act on the blood vessels) and toxins that alter the shape of red blood cells.
Myotoxins:- are toxins which break down muscle cells. They are usually PLA type molecules. Myoglobin from the muscle cells leaks into the blood and can cause myoglobinuria.
The chemical proteins and enzymes that have been identified so far are:
- L-arginine ester hydrolases, which breakdown the bodies amino acids.
- Hyaluroniclase, which effects the hyaluronic acid production vital for connective tissue in the body.
- L-amino acid oxidase, which also breakdown the bodies amino acids.
- Cholinesterases destroy or block acetylcholine thus interfering with neurotransmission.
- Phospholipases, which destroys phospholipids essential for cell walls.
- Ribo and deoxyribonucleic oxidases, essential for the manufacturing of genetic material in the body.
- ATPases, essential for energy production of cells within the body.
Snake Venom: Methodology in Determining Antivenom Treatment
As a medical scientist, one of my duties is to perform the venom identification testing on specimens, both animal and human, so that the correct antivenom treatment can be administered or in the case of livestock, insurance claims can be processed.
At present, the Commonwealth Serum Laboratory (CSL) manufacture the only detection kit that is a rapid Enzymic Linked Immuno Sorbent Assay (ELISA) that takes approximately 25 minutes to perform. The kit is useful in identifying the correct antivenom to use in snake bites in Australia and Papua New Guinea. Specimens can be collected via bite site swabs in urine, blood or bodily tissue. In the detection process as a medical scientist, I have found that urine specimens are more accurate than blood as red cells from whole blood can give false positive readings if the reaction wells are not fully washed properly during the wash stage of the kit. Swabs may detect venom but envenomation may not necessarily have occurred.
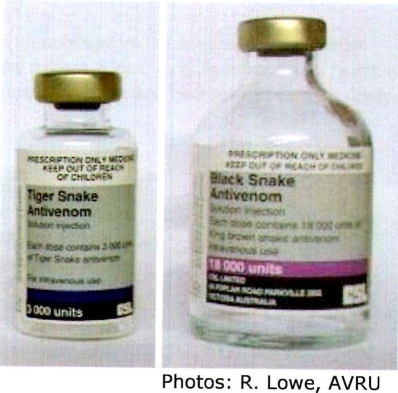
It is very important not to administer antivenom until venom has been detected, and the correct monovalent, i.e. serotype specific antivenom, can be administered. If the patient has been bitten and clearly showing signs of envenomation, a multipurpose polyvalent antivenom can be used. If identification is to be delayed, however, there may be some adverse effects. Dosages are usually required in higher amounts.
 The kit categories include five monovalent antivenoms each of which contain a number of snake venoms that the antivenom neutralises. These are as follows:-
The kit categories include five monovalent antivenoms each of which contain a number of snake venoms that the antivenom neutralises. These are as follows:-
Tiger Snake: intended to neutralise Tiger Snake (Notechis scutatus), Copperhead (Austrelaps superbus), Red-bellied Black Snake (Pseudechis porphyriacus), and the Clarence River or Rough Scaled Snake (Tropidechis carinatus).
Brown Snake: intended to neutralise Brown Snake (Pseudonaja textilis), Dugite (Pseudonaja affinis), and the Gwardar (Pseudonaja nuchalis).
 Black Snake: intended to neutralise King Brown or Mulga Snake (Pseudechis australis), Papuan Black Snake (Pseudechis papuanis), and the Red-bellied Black Snake (Pseudechis porphyriacus).
Black Snake: intended to neutralise King Brown or Mulga Snake (Pseudechis australis), Papuan Black Snake (Pseudechis papuanis), and the Red-bellied Black Snake (Pseudechis porphyriacus).
Death Adder: intended to neutralise Death Adder (Acanthophis antarcticus), and the Desert Death Adder (Acanthophis pyrrhus).
 Taipan: intended to neutralise Taipan (Oxyuranus scutellatus) and the Small Scaled or Fierce Snake (Oxyuranus microlepidotus).
Taipan: intended to neutralise Taipan (Oxyuranus scutellatus) and the Small Scaled or Fierce Snake (Oxyuranus microlepidotus).
The principal of the test is that a colour change will develop in a ‘well’ of the required antivenom thus allowing the choice of a specific monovalent antivenom.
Antivenom is made by administering horse blood with snake venom in small amounts, which causes an immunological response by the blood to develop antibodies against the venom. The serum proportion of blood is then separated and freeze-dried. The product is reconstituted (liquefied) prior to use.
Snake Venom: References:
Bohinski, R.C. (1987), Modern concepts in Biochemistry, 5th Edition, Allyn & Bacon Inc, Massachusetts, USA.
Brazaitis, P. & Watanabe, M.E. (1992), Snakes of the world, Michael Friedman Publishing Group, New York, USA.
Curtis, H. (1983), Biology, 4Ih Edition, Worth Publishers inc, New York, USA.
Ehmann, H. (1992), Encyclopedia of Australian Animals; Reptiles, Angus & Robertson Publishers Pty Ltd, Sydney, Australia.
Rang, H.P., Dale, M.M., & Ritter, J.M.(1993), Pharmacology, 3rd Edition, Churchill Livingstone, Edinburgh, Scotland.
Shine, R. (1994), Australian Snakes a natural history, Revised Edition, Reed Books, Chatswood, Australia.
Slater, P. (1997), Amazing Facts about Australian Frogs and Reptiles, discover and learn, vol4, Steve Parish Publishing Pty Ltd, Fortitude Valley, Australia.
Snake Venom Detection Kit; (kit insert), (1999), CSL Biosciences Department, Parkville, Australia.
Mirtschin,P. J., Masci, P., Paton, D. C., Kuchel, T. (1998).
Snake bites recorded by veterinary practices in Australia. Aust Vet J. 76: 3 195-1 98
Sutherland, S.K. (1992). Deaths from snake bite in Australia, 1981 -1 991. Med. J. Aust.. 157: 740-746 Sutherland, S. K. (1991). Snake Bites Patient Management Guide ERR: 62-63
Sutherland, S. K. (1990). Treatment of snake bite. Aust. Family Physician. 19: 1 1-1 3
Sutherland, S. K. (1974). Venomous Australian creatures: The action of their toxins and the care of the envenomated patient. Anaesth. Intens. Care. 11 :4: 31 6-328
Sutherland, S. (1983). First aid management of snakebite. Med. J. Aust. Feb 5: 106.
Sutherland S. K., Duncan, A. W. (1980). New first-aid measures for envenomation. Med. J. Aust. April 19: 378- 379.
Sutherland, S. K., Coulter, A. R., Harris, R. D. (1979). Rationalization of first-aid measures for Elapid snakebite. The Lancet . Jan. 27: 183-1 86
Snake Venom
 First aid for tiger snake envenomation consists of a pressure bandage and immobilisation. In cases where a pressure bandage has been applied correctly, it can be left in situ indefinitely while the patient is feeling no discomfort as a result. If it becomes appropriate to remove a pressure bandage, it is necessary to have antivenom and haemostatic support ready. In severe cases, a patient may require ventilatory support.
First aid for tiger snake envenomation consists of a pressure bandage and immobilisation. In cases where a pressure bandage has been applied correctly, it can be left in situ indefinitely while the patient is feeling no discomfort as a result. If it becomes appropriate to remove a pressure bandage, it is necessary to have antivenom and haemostatic support ready. In severe cases, a patient may require ventilatory support.